Early Functional Rehabilitation with the Happiness Programme at University Hospital Southampton.
The ICU Physiotherapy and Occupational Therapy team at NHS University Hospital Southampton have been using the Happiness Programme with patients in their General Intensive Care Unit. Lucy from the team wrote about one patient’s experience of using the Happiness Programme to support functional rehabilitation and presented it at the 8th European Conference on Weaning and Rehabilitation in Critically-ill Patients. She has kindly given us permission to share her findings.
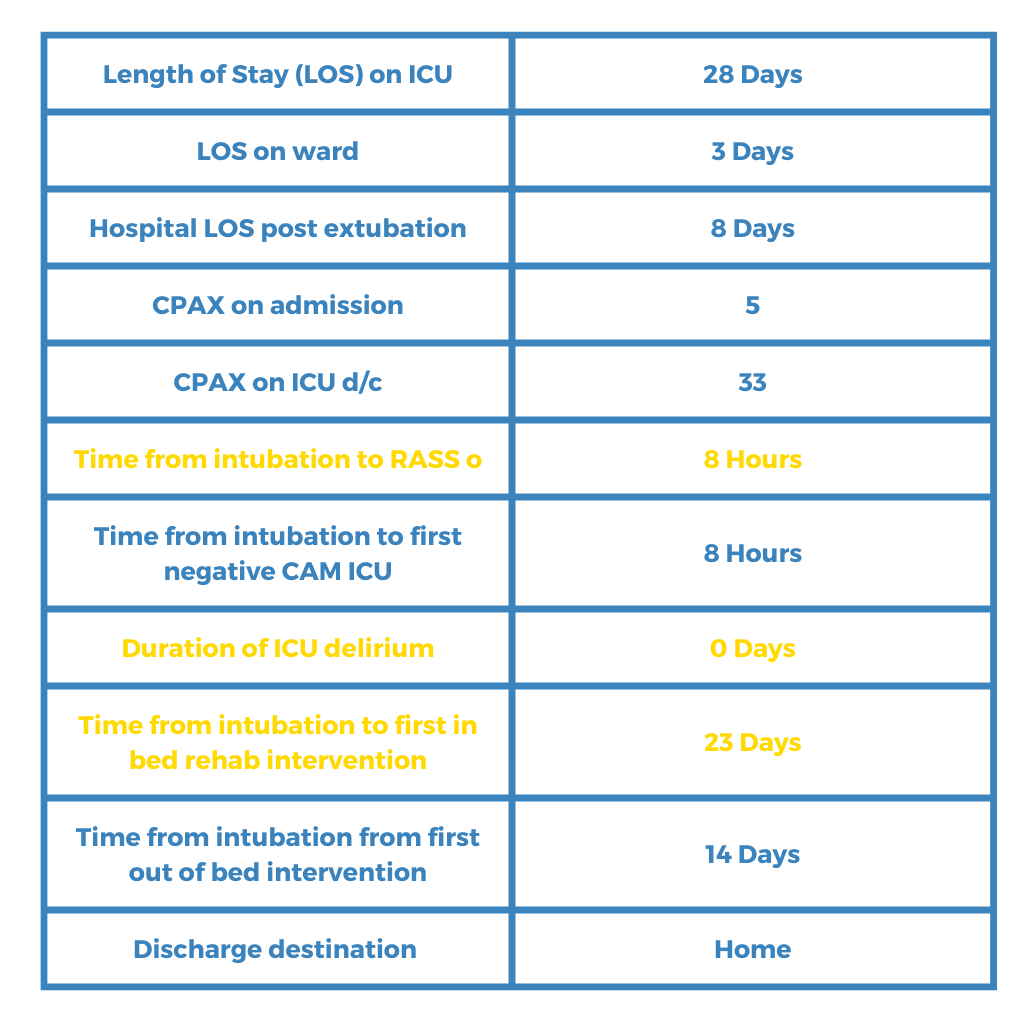
Outcomes
As a result of utilising the Happiness Programme to support functional rehabilitation, Lucy and her team found the following:
Reduced risk of ICU acquired delirium
Reduced hospital length of stay
Maximised independence
Introduction
A 76 year old female was admitted to General Intensive Care Unit (GICU) following exacerbation of asthma, requiring intubation and ventilation (I+V) via endotracheal tube (ETT). Due to a subglottic mass affecting her airway she was unable initially to be successfully intubated or ventilated by tracheostomy, resulting in her being I+V via ETT for over 3 weeks.
Due to her being difficult intubation and to reduce the risk of airway complications out of bed rehab was no initially completed, however the MDT decision was made to reduce sedation to allow the patient to participate in bed rehab to reduce the risk of developing physical and non physical morbidities of critical illness outlined in National Institute for Health and Care Excellence (NICE) QS158.
Functional Rehabilitation
Sedation was adjusted to achieve Richmond Agitation-Sedation Scale (RASS) of 0 to allow for rehabilitation.
A person-centred functional approach was adapted for her rehabilitation to reduce risk of ICU acquired delirium and increase engagement.
“Patient profile” was used to guide meaningful conversations and activities within rehabilitation.

As the patient was a keen cyclist virtual motomed routed and a map to progress her “journey home”.
Functional upper limb (UL) rehabilitation to achieve goals of independent personal care tasks and to establish a communication method.
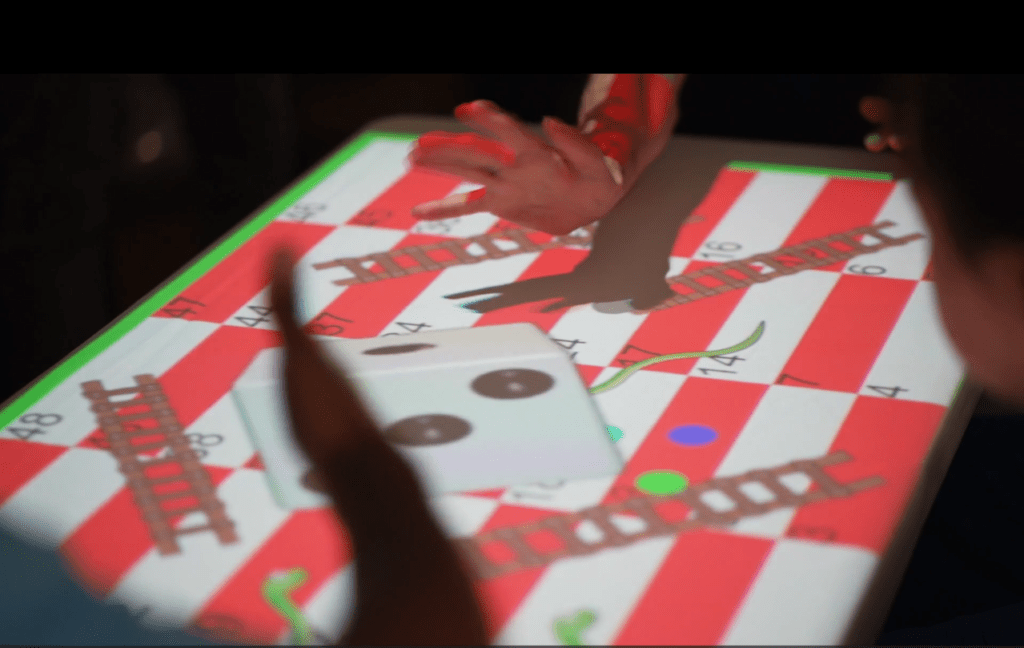
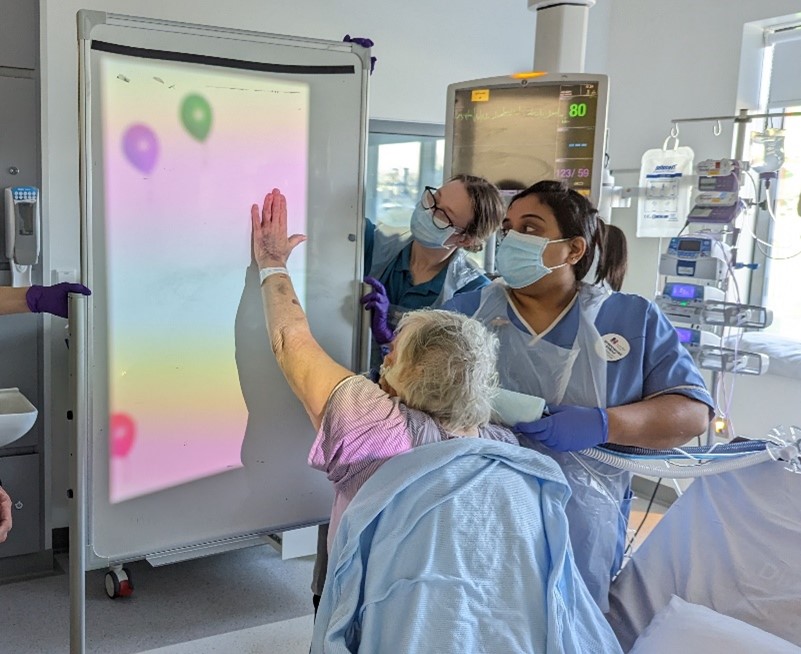
Cognitive stimulation through games and puzzles to reduce risk of ICU delirium.
To humanise her rehabilitation and reduce the risk of psychological impact of critical illness the therapy team completed activities focussing on wellbeing including hair washing and painting nails.
As well as progressing mobility, interactive games projected onto a white board to challenge standing tolerance and dynamic balance.
Personal care activities were graded and progressed resulting in patient being able to shower with minimal assistance the day after extubation.
“I really enjoyed the interactive games… it was a nice change and nice to do something different.” - Patient at UHS
Results
Conclusion
Optimum sedation to allow a person-centred functional approach to rehabilitation, in this care, appears to have reduced the risk of ICU acquired delirium, reduced hospital length of stay and maximised independence.
Despite the delay to out of bed rehabilitation this patient was independently mobile with zimmer frame, independent with all transfers, independent on the stairs and independent with personal care 8 days post extubation.
The patient commented that she felt she gained some control back by being able to communicate and do things for herself. She remained fully engaged and motivated in her rehab throughout her stay on GICU.
Lucy's Poster